
Am I the only one with GI issues?
Gastro-intestinal complaints are very common amongst endurance athletes with an estimated 30 to 50% of distance runners experience intestinal problems related to exercise.
What are the most common issues?
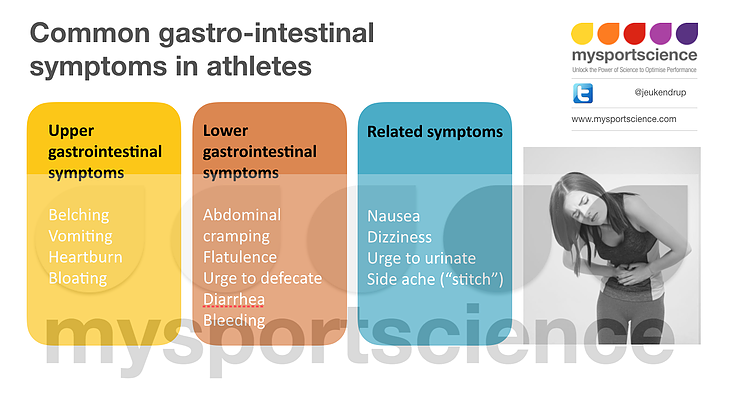
The complaints are normally divided into two primary categories: symptoms of the upper intestinal tract or symptoms of the lower intestinal tract (see figure). The most common upper GI symptoms include: ructation (belching) and vomiting, abdominal pain, gastroesophageal reflux (or heartburn), and bloating. Lower GI symptoms include: abdominal pains and cramping, increased flatulence, urge to defecate, and loose stool, diarrhea or even bloody diarrhea.
There is a third category of symptoms that cannot be classified as upper or lower gastro-intestinal problems but might be related to the gastro-intestinal tract (for example stitch).
All of the symptoms may be experienced in any sport. In triathlon the symptoms are more common during the run segment as this occurs later in the race and is physiologically the most demanding of the three activities.
Why do these GI problems occur?
At present, the causes of gastrointestinal symptoms are not completely understood. The symptoms are difficult to investigate because they are often specific to race situations and are very difficult to reproduce or simulate in a laboratory. Nevertheless, some laboratory studies have been performed. From these studies, a number of potential causes and contributors have been identified and they can be divided into 3 general categories: mechanical, physiological and nutritional.
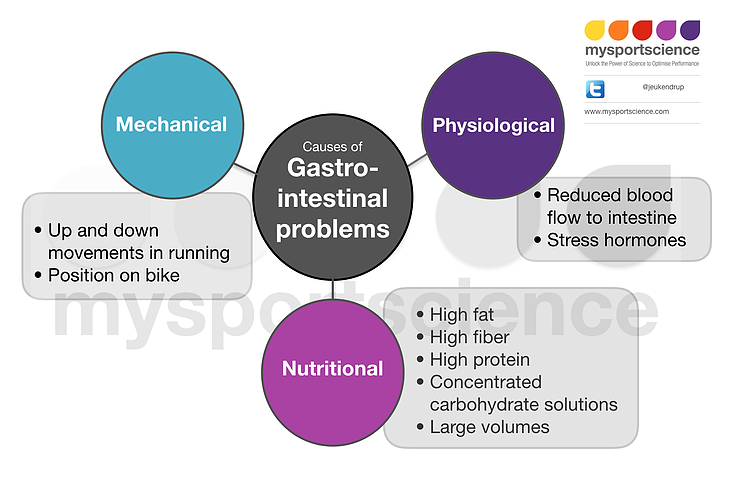
Mechanical causes
The mechanical causes of GI-problems are either impact-related or are related to posture.
In sports like running, repetitive high-impact mechanics are thought to be implicated in multiple issues. Gastrointestinal bleeding is common amongst runners and is thought to be symptomatic of damage to the intestinal walls due to repetitive impact. As well, this repetitive bouncing of the GI tract during running is thought to contribute to lower GI symptoms such as flatulence, diarrhea and urgency.
Posture can also have an effect on GI symptoms. For example, on a bicycle (especially in aero position), upper GI symptoms are more prevalent possibly due to more horizontal position and increased pressure on the abdomen. Further, "swallowing" air with water bottles and aggressive cycling posture can result in mild to moderate stomach distress.
Physiological causes
Physiological causes of GI-symptoms include reduced blood flow and increased anxiety (especially before competition).
With exercise, blood flow is preferentially redirected to the working muscles and blood flow to the gut can be reduced by as much as 80%. Such low blood supply can compromise gut function to varying degrees and can result in commonly experienced GI symptoms such as cramping.
Anxiety has an effect on hormone secretion which in turn can affect gut movement, resulting in incomplete absorption and loose stool.
Nutritional causes
A wide variety of nutrition factors can have strong influence on gastro-intestinal distress. Fiber, fat, protein, and fructose have all been associated with a greater risk to develop GI-symptoms.
Dehydration, possibly as a result of inadequate fluid intake, may also exacerbate the symptoms.
Beverages with high carb density seemed to be responsible for some of the reported complaints (typically issues occur with drinks containing >12 g/100 ml of carbohydrate as well as electrolytes; most sports drinks are around ~6 g/100 ml).
Dairy products may also be linked to the occurrence of gastrointestinal distress as a result of even mild lactose intolerance; this can result in increased bowel activity and mild diarrhea.
How can I prevent these GI issues?
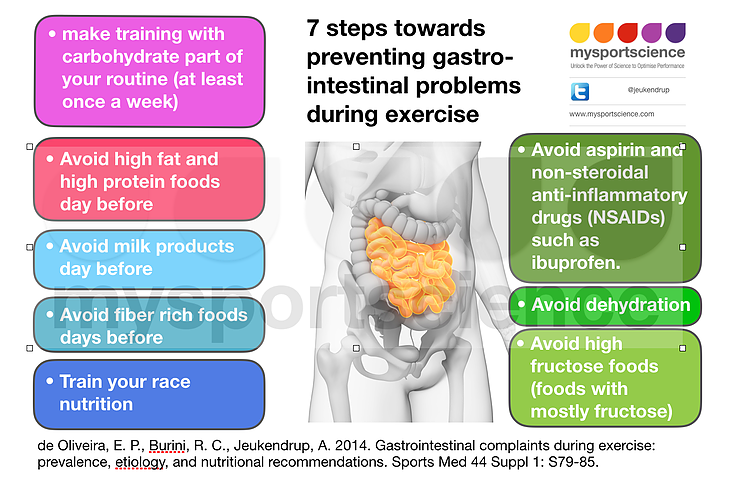
There are at least 7 steps you can take to prevent GI issues whether caused by mechanical, physical, or nutritional issues. Not all suggestions will work for everyone, but hopefully every sufferer can find one or two that do help address their specific issues. The guidelines below are based on limited research, but anecdotally these guidelines seem to be effective:
- Avoid high fiber foods the day or even days before competition. While fiber is generally important to keep the bowel regular, fiber before race day is different. Fiber can increase need for bowel movements during exercise, accelerate fluid loss, and may result in unnecessary gas production (resulting in cramping).
- Avoid aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen. Both have been shown to increase intestinal permeability and may increase the incidence of GI complaints.
- Avoid milk products in the day or days leading up to a race as even mild lactose intolerance can cause problems during exercise.
- Avoid fructose-only foods. Fructose is absorbed by the intestines more slowly the tolerance of fructose is much less than glucose (may lead to cramping, loose stool and diarrhea). Note that fructose in combination with glucose may not cause problems and may even be better tolerated (see the full blog here).
- Avoid dehydration as it can exacerbate symptoms of any GI issues.
- Practice new nutrition strategies so that you are comfortable executing the plan mechanically and ensure your body is trained to handle that level of intake.
- Train your gut so that it can up-regulate to handle the levels of intake.
For more details and additional references, please see these blogs from Asker’s blog on www.mysportscience.com





